TOC |
Cardiology
TOC |
Cardiology

See * PERIOPERATIVE POCKET MANUAL
REF: Lowering Cardiac Risk in Noncardiac
Surgery -
NEJM Dec.
6, 2001 Lee Fleisher, Kim Eagle
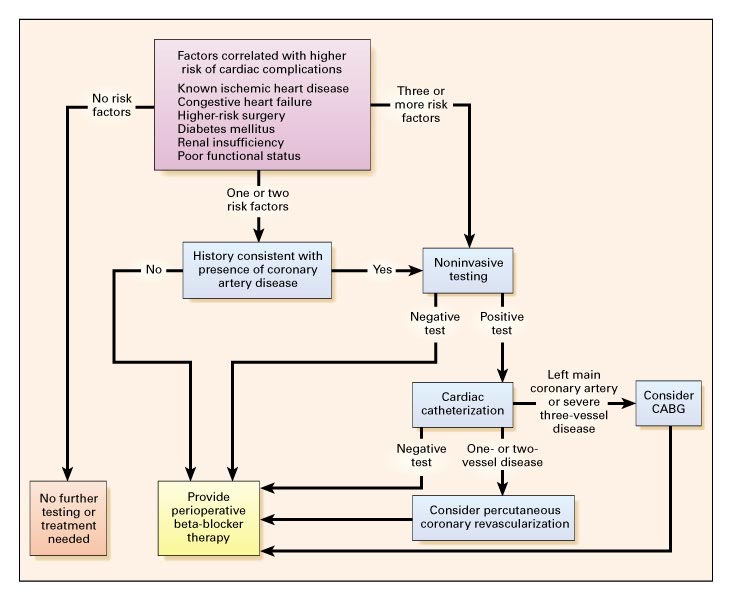
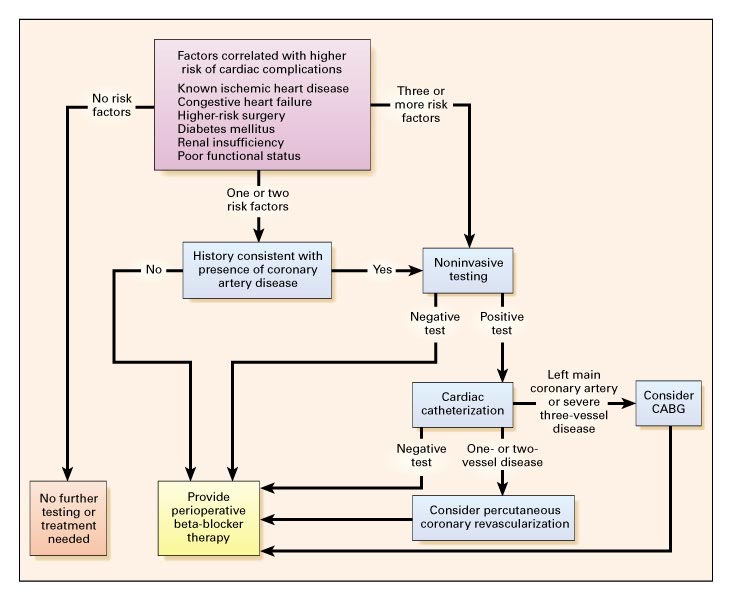
The history and findings on physical examination may identify other conditions
that place the patient at high perioperative risk and should lead to further
consideration of additional diagnostic procedures.
Patients with no cardiac risk factors are generally at very low risk and
need no further evaluation or therapy.
Asymptomatic patients who have one or more risk factors for coronary disease
(e.g., a family history of coronary heart disease, smoking, an elevated
cholesterol level, obesity, or inactivity) but who do not have established
coronary artery disease have been shown to be at very low risk. An exception
is patients with diabetes, particularly long-standing diabetes.
Factors that increase the risk of Perioperative
Cardiac Complications in Patients Undergoing Noncardiac Surgery & Indications
for the Use of Perioperative Beta-Blocker Therapy:
-
Ischemic heart disease - yes on Beta-Blocker Rx
-
Congestive Heart Failure - yes on Beta-Blocker Rx
-
High-risk surgery - Probably yes on Beta-Blocker Rx
-
Diabetes mellitus (esp. on insulin Rx) - yes on Beta-Blocker Rx
-
Renal insufficiency - Uncertain on on Beta-Blocker Rx
-
Poor functional status - - yes on Beta-Blocker Rx if CAD or CHF patients
Beta-Blockers and Reduction of Cardiac Events in Noncardiac Surgery
Clinical Applications - Andrew D. Auerbach; Lee Goldman
JAMA.
March 20, 2002;287:1445-1447
[Although current evidence describing the effectiveness of perioperative
Beta-blockade may not address all possible clinical situations, it is possible
to formulate an evidence-based approach that will maximize benefit to patients.
We describe how information from several sources can be used to guide management
of patients with limited exercise tolerance, those at highest risk for
perioperative cardiac events, patients who are taking Beta-blockers long-term,
and those with relative contraindications to Beta-blockade. Even though fine
points of their use remain to be elucidated, perioperative Beta-blocker use
is important and can be easily applied in practice by any physician involved
with the care of patients perioperatively.]
Therapies and Interventions to Reduce Perioperative
Cardiac Complications fall into three categories:
-
preoperative coronary revascularization
include percutaneous coronary intervention with balloon angioplasty,
with or without the placement of coronary stents, and coronary-artery bypass
grafting.
-
perioperative medical therapy
include Beta-blockers, Alpha2-adrenergic agonists (as clonidine or
Mivazerol), nitrates (nitroglycerin), and calcium-channel blockers (as
diltiazem). Other agents, such as aspirin, angiotensin-converting–enzyme
inhibitors, and statins, play an important part in the treatment of
cardiovascular disease.
-
intraoperative and postoperative monitoring.
Strategy for Assessing the Risk of Perioperative
Coronary Complications in Patients Scheduled to Undergo Noncardiac Surgery:
Perioperative Management of Diabetic Patients
-
Review
Arch IM Nov.8, 1999;159:2405 - Scott Jacober, James Sowers
In general, the goal for glucose control during surgery is to maintain
the glucose level between 8 and 11 mmol/L (approximately 150 and 200
mg/dL) during surgery to protect against hypoglycemia.
Type 2 Diabetes Treated With Oral Antidiabetes Agents
For patients treated with oral agents, these agents are generally administered
on the day before surgery and withheld on the day of surgery. If patients
manifest marked hyperglycemia, supplemental insulin can be administered to
achieve better glycemic control, and the surgery may be performed if electrolyte
levels are acceptable. Hyperglycemia during the perioperative period
in patients previously treated with these agents should be corrected with
insulin.
Sulfonylureas are routinely continued on the day before surgery and
withheld on the operative day.
Metformin (The biguanide) is discontinued on the day of surgery
because complications or alterations in renal function arising intraoperatively
may potentiate the risk of development of lactic acidosis. The
biguanide should not be resumed for 72 hours postoperatively, when serum
creatinine is measured to document the absence of dye-induced renal toxic
effects and normal renal function.
Thiazolidinediones are not insulin secretagogues and may be discontinued
on the day of surgery.
Type 1 or Type 2 Diabetes Treated With Insulin
Many patients who use insulin can be treated with conventional subcutaneous
insulin therapy. For individuals who take long-acting insulin (ie,
extended insulin zinc [Ultralente]) and short-acting insulin, a switch to
an intermediate-acting type a day or two before planned surgery is
appropriate.
Subcutaneous Insulin Regimens
(Figure
3).
Preoperative insulin recommendations are much more complex and require more
logistic contingencies
(Figure
3).
For early-morning procedures of short duration where the patient may still
be expected to eat according to his or her usual meal plan, it is easiest
to give the morning insulin and food after the procedure. Shortening the
intervals between later meals may compensate for this delay and gradually
realign the patient's mealtimes back to the usual schedule. This operative
schedule is the easiest for patients and physicians because it has the least
disrupting effect on the diabetes regimen and should be advocated by both
patient and the physician responsible for managing the diabetes.
If the surgery can be performed in the morning, but it is likely that
the breakfast meal will be omitted, preoperative insulin should be administered.
If the patient is treated with a single morning dose of intermediate-acting
insulin, then two thirds of that dose should be administered in the morning
as intermediate-acting insulin if the patient is likely to eat lunch. If
the patient is treated with a twice-daily dose of insulin, then one half
of the total morning dose (including short-acting insulin if prescribed)
should be administered in the morning as intermediate-acting insulin. If
the likelihood of consuming lunch is low, one half of the total morning dose
(including short-acting) should be administered as intermediate-acting insulin
for the patient treated with a single dose of insulin and one third for a
twice-daily regimen. For those on a regimen of morning intermediate-acting
and short-acting insulin, short-acting insulin at supper, and bedtime
intermediate-acting insulin, recommendations are similar to those for the
twice-daily insulin regimen. For the patient who is taking multiple doses
of short-acting insulin (MDI regimen) one third of the premeal dose of
short-acting insulin is administered at the appropriate time. Patients treated
with continuous insulin infusion therapy (insulin pumps) may be treated with
their usual basal infusion rate.
When surgery is scheduled later in the day, more complex modifications
are frequently necessary, and an intravenous infusion of glucose is recommended
at 5 g/h. For individuals previously treated with a single dose of
insulin, one half of the total dose of morning insulin should be given as
intermediate-acting insulin in the morning. For those treated with 2 or 3
doses, one third of the morning total dose is given as intermediate-acting
insulin. Patients taking multiple doses of short-acting insulin may receive
one third of the morning dose of short-acting insulin and one third of the
lunch dose of short-acting insulin at the appropriate time.
Intravenous Insulin Regimens
Intravenous regular insulin is indicated during the perioperative period
for previously insulin-treated patients undergoing long, complex operative
procedures; patients who require emergency surgery while in ketoacidosis;
and patients with unstable type 1 diabetes.
Guidelines for perioperative cardiovascular
evaluation for noncardiac surgery
Report of the Am. College of Cardiology/Am.
Heart Association Task Force on Practice Guidelines 1996 Mar 15.
Perioperative cardiovascular evaluation
Step-by-step approach to risk assessment and follow-up care
Arsad A. Karcic, MD; Mohammed K. Rizvon, MD
VOL
108 / NO 6 / NOVEMBER 2000 / POSTGRADUATE MEDICINE
Approach
to Peri-operative Care JCOM August 2000
Lowering Cardiac Risk in Noncardiac
Surgery -
NEJM Dec.
6, 2001 Lee Fleisher, Kim Eagle
Beta-Blockers and Reduction of Cardiac Events in Noncardiac Surgery
Clinical Applications - Andrew D. Auerbach; Lee Goldman
JAMA.
March 20, 2002;287:1445-1447
Preoperative Evaluation of the Patient With Hypertension
JAMA
April 24, 2002;287:2043 Lee A Fleisher


04172002